What is Keratoconus?
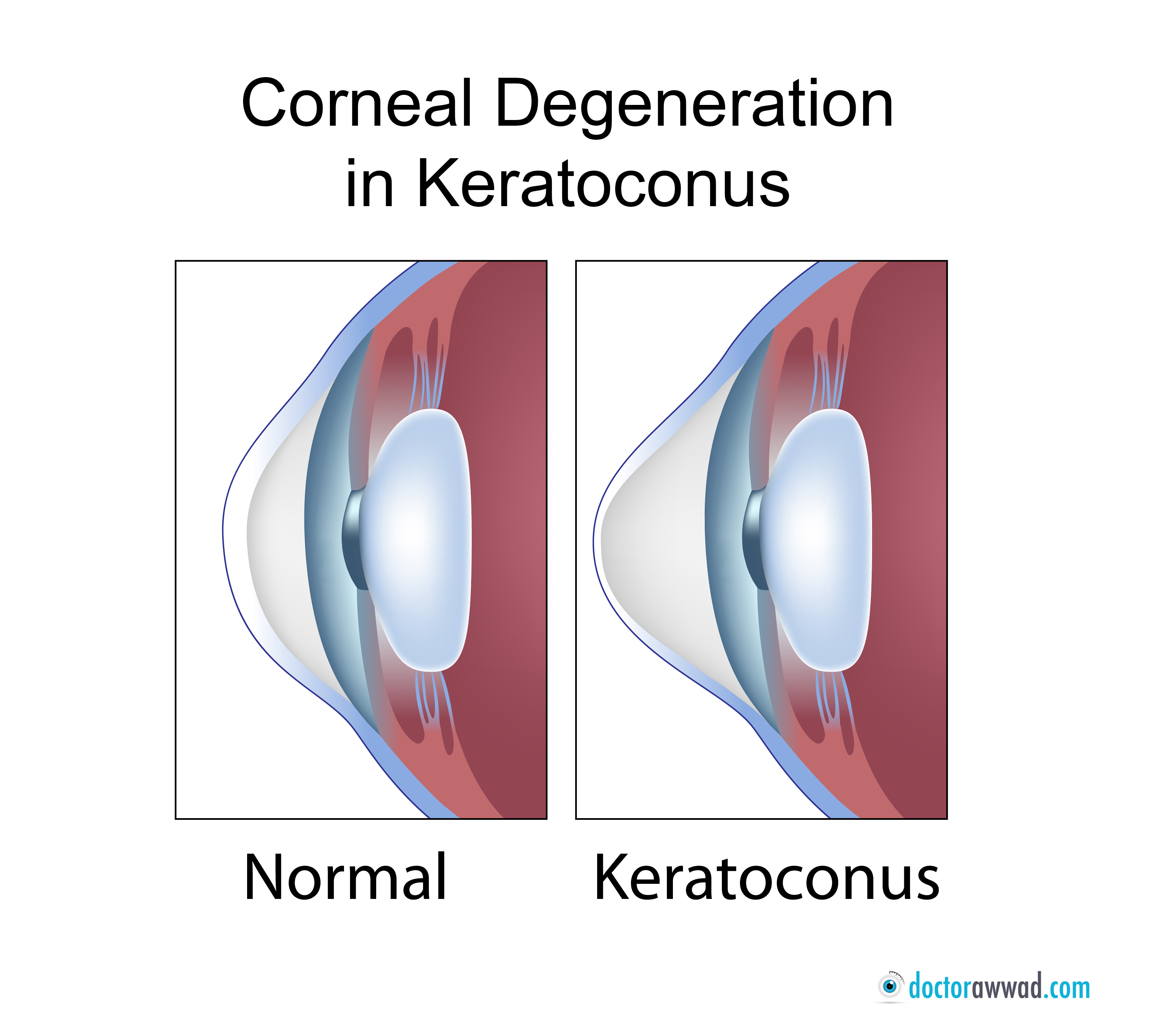
Keratoconus is a disease that affects the clear transparent front portion of the eye known as the cornea, leading to corneal weakening and irregular forward protrusion and thinning (Picture). The resultant abnormal corneal shape leads to irregular astigmatism and visual degradation, which typically does not improve fully upon correction with eyeglasses. Affected individuals usually complain of blurred vision and distorted contours and shadows around objects, even while wearing their eyeglasses.
What leads to Keratoconus?
What leads to Keratoconus is not fully understood yet. Multiple factors seem to be involved, in part or in total, for the development of the disease. Genetic predisposition is important, as a good proportion of affected individuals have relatives suffering from the same condition. Other factors include allergy and eye rubbing, the latter being regarded as an important factor in the development and progression of the disease.
Keratoconus typically starts during teenage-hood, but it can sometimes manifest even earlier, as early as 5 years of age. The disease tends to worsen between late teens and mid twenties, then it slows down and stabilizes in the mid to late 30s. Keratoconus does not usually worsen after the age of 40. Affected individuals first experience a progressive and sometimes rapid worsening in their refractive (visual) error, mainly leading to an increase in astigmatism, but also in myopia. Often, one eye tends to be affected more than the other. A careful eye examination and a corneal topography measurement can help diagnose the condition.
Non surgical
A point might be reached when the spectacles would not correct vision fully, with distorted contours and blurred vision persisting even with eyeglasses. At this stage, vision could improve significantly if hard or hybrid contact lenses are worn daily. Lubrication with artificial tears and punctual plugs inserted in the eyelids can improve patients tolerance for hard and hybrid lenses.
Corneal ring segments
Many patients might be intolerant to hard or hybrid contact lenses due allergy, eye dryness, and mechanical rubbing between the steep corneal shape and the lens. At this stage, plastic ring segments known as intrastromal corneal ring segments might be inserted in the cornea using laser technology in order to flatten and regularize corneal shape, and subsequently, improve vision. Intrastromal corneal ring segments are small arc-like pieces made of plastic material that can be found in intraocular lenses placed during cataract surgery. Channels are created in the cornea using a specialized femtosecond laser system. The corneal ring segments are inserted through the laser-created channels. Once in, the cornea tends to flatten and regularize within a few days and up to 6 months. Vision subsequently improves, as does the refractive error. The improvement from the intrastromal corneal ring segments, however, is not necessarily total, and is not always guaranteed. Studies have shown that around 80% of patients do improve significantly. Improvement is defined by better vision and visual quality with or without eyeglasses, a lower refractive error in terms of myopia and astigmatism, or less or no dependency on hard or hybrid contact lenses. Some patients, previously intolerant to hard/hybrid lenses, get to tolerate them again due to corneal flattening and improvement in corneal shape.
Additionally, corneal ring segments insertion procedure is safe and reversible. It is a short and easy procedure performed in the laser suite, under local topical anesthesia. Patients can resume normal activity one or two days later, and their vision usually improves over the next several days and up to 6 months. Corneal rings are hardly noticeable on casual looks, but might be apparent for the astute observer on close-up examination. Ring segments do not usually stop disease progression; they mainly enhance corneal shape, decrease visual errors, and improve vision.
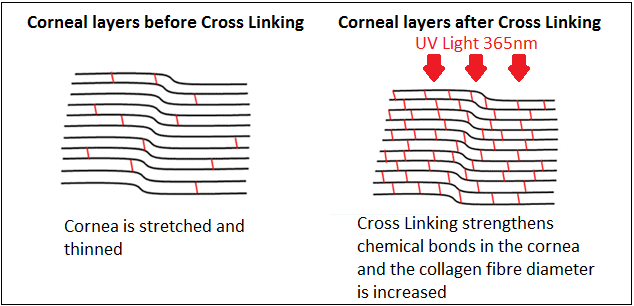
Corneal cross-linking
To stop disease progression, one procedure has been proven effective: ultraviolet corneal cross-linking. In Corneal cross-linking, riboflavin (vitamin B2) eye drops are instilled in the eye followed by exposure to a focused ultraviolet light. The combination of the UV light and riboflavin drops produces a reaction inside the cornea, which helps cross-linking corneal macromolecules, and hence, strengthens the cornea and makes it stiffer. A stiff cornea resists further protrusion and thinning and puts a stop to disease progression. Cross-linking works most of the time. Even though the aim of cross-linking is to stabilize the disease process and maintain vision, some patients experience an improvement in vision and a decrease in refractive error. Full visual recovery after corneal cross-linking might take a few weeks and sometimes a few months. Only a very small percentage of patients might experience a final slight worsening in vision after the procedure. Corneal cross-linking is usually offered to patients with documented disease progression and in all affected individuals who are younger than 19 years, as the majority of them have been shown to experience worsening and disease progression. Cross-linking is performed under anesthetic drops and is a comfortable procedure.
Additional surgical interventions
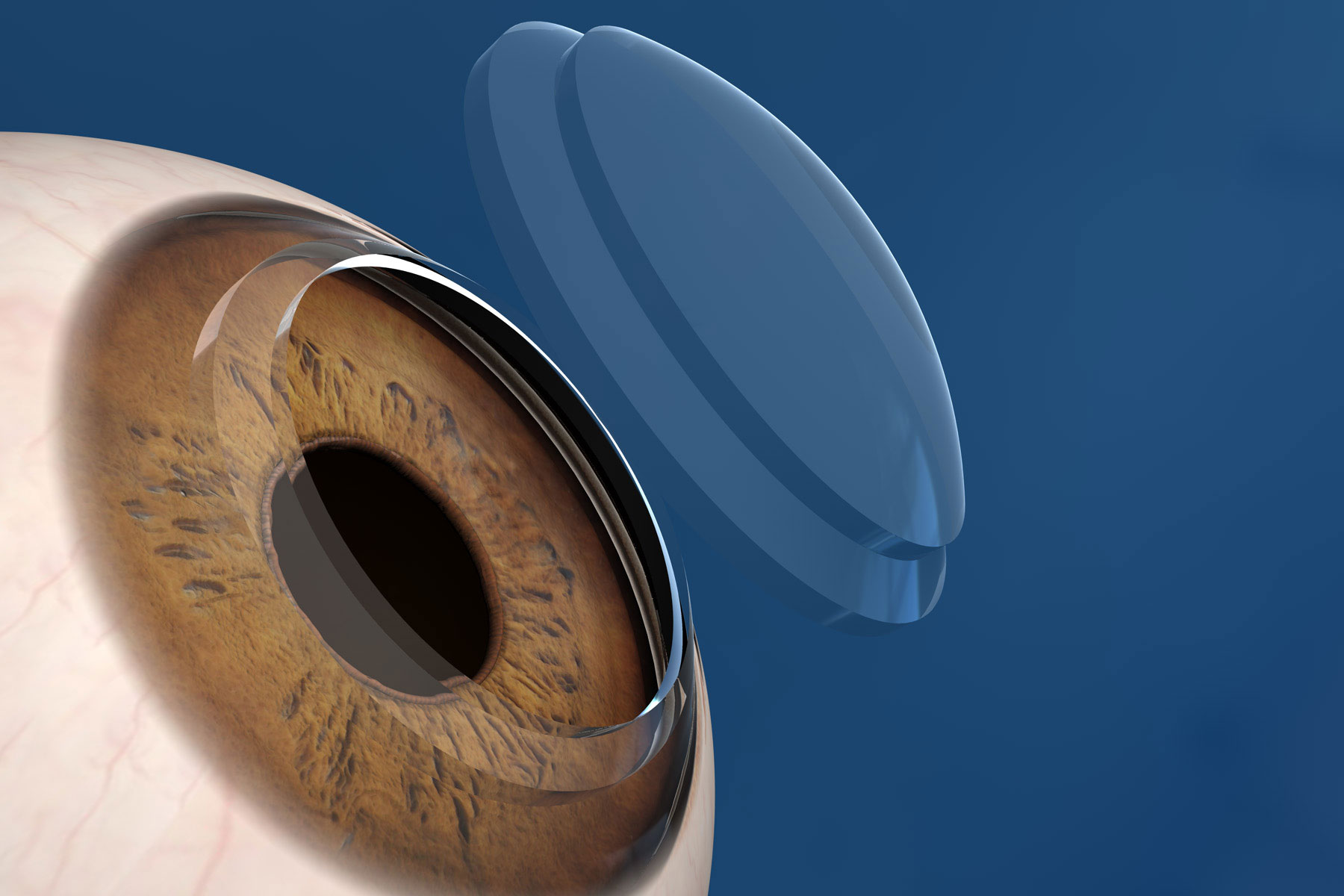
LASIK and laser surface ablation are generally contra-indicated in keratoconus patients. However, in certain situations, customized minimal laser surface ablation or PRK, combined with or performed after UV cross-linking, can improve vision. Additionally, patients with stable disease and enjoying an acceptable visual acuity with their eyeglasses can be sometimes candidates for implantable corrective lens procedure (ICL), which could minimize and often eliminate the dependency on spectacles. Patients suffering from poor vision, intolerant to hard or hybrid contact lenses, and not candidate for ring segment insertion (or having failed to improve after the procedure) might benefit from corneal transplantation. Successful outcome is expected in 90 to 95 % of young keratoconus patients. Full visual recovery, however, might take up to a year to be attained. Risks include corneal graft rejection and graft failure. A small percentage of patients might still need to be fitted with hard or hybrid lenses even after corneal transplantation.
What to do when an individual is diagnosed with keratoconus? Two targets should be in mind: vision enhancement and vision stabilization. First, vision enhancement: If eyeglasses fail to improve vision, then hard or hybrid contact lenses should be tried. In case of intolerance, then corneal ring segments are indicated to optimize vision. Customized laser surface treatment combined with cross-linking can help in improving vision in some patients, even after ring segment placement. Second: vision stabilization. If age is below 40, a corneal topography and an eye exam need to be performed every 6 months to one year to ensure disease stability. If disease progression is documented, whether on initial or on subsequent examinations, then corneal cross-linking is mandatory. If the affected individual is younger than 19 years, a corneal cross-linking is indicated regardless of documented disease progression.
As a summary of interventional measures to improve vision, if eyeglasses correct vision satisfactorily, no further modality is sought. If vision remains blurry even with spectacle wear, a trial of hard or hybrid lenses is initiated. If the latter could not be tolerated, then corneal ring segment insertion procedure is indicated. Meanwhile, regular follow-ups should be scheduled and corneal cross-linking can be performed at any stage if disease progression is documented. If all fails, corneal transplantation is performed to restore sight. Your eye doctor should guide you on which treatment modality is right for you and when to schedule your next follow up appointment to monitor disease progression.